RECURRENT MISCARRIAGE
☺

DEFINITION :
” Recurrent miscarriage is defined as the sequence of two or more spontaneous abortion as documented by either sonography or on histopathology , before 20 weeks “
INCIDENCE :
- This distressing problem is affecting approximately 1% of all women of reproductive age
- The risk increase with each successive abortion reaching over 30% after three consecutive loses
ETIOLOGY :
The etiology (causes) of recurrent miscarriage can be complex and multifactorial…..
- Genetic Factors: Chromosomal abnormalities in either parent can contribute to miscarriages. This includes structural abnormalities in chromosomes or numerical abnormalities (e.g., trisomies).
- Anatomical Factors: Issues such as uterine abnormalities (like septate uterus or intrauterine adhesions), cervical incompetence (inability of the cervix to stay closed during pregnancy), or fibroids can increase the risk of miscarriage.
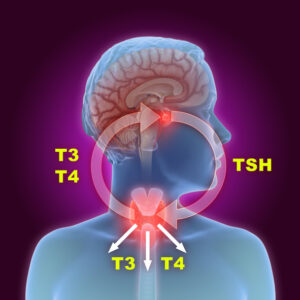
- Hormonal Factors: Imbalances in hormones crucial for pregnancy maintenance, such as progesterone and thyroid hormones, can lead to miscarriage.
- Immunological Factors: Some autoimmune disorders or immune system abnormalities may lead the body to attack the developing embryo or fetus.
- Infections: Certain infections, such as cytomegalovirus (CMV), toxoplasmosis, or bacterial infections, can increase the risk of miscarriage.
- Lifestyle Factors: Factors such as smoking, excessive alcohol consumption, drug use, and obesity can contribute to recurrent miscarriages.
- Thrombophilic Disorders: Conditions that increase the tendency to develop blood clots, such as antiphospholipid syndrome, can lead to miscarriage by affecting blood flow to the placenta.
- Environmental Factors: Exposure to certain environmental toxins or chemicals may increase the risk of miscarriage.
- Advanced Maternal Age: Women over the age of 35 are at higher risk of miscarriage due to increased chromosomal abnormalities in eggs.
- Paternal Factors: Abnormal sperm parameters or genetic factors in the father can also contribute to recurrent miscarriages.
CLINICAL FEATURE :
The clinical features and characteristics associated with recurrent miscarriage can vary, but generally include the following:
- Repetitive Pregnancy Loss: The hallmark feature is the recurrence of miscarriages, typically defined as three or more consecutive losses. These losses may occur at different stages of pregnancy but typically before the 20th week.
- Timing of Miscarriages: Recurrent miscarriages often occur in the first trimester (before 12 weeks), but they can also occur in the second trimester (between 12 and 20 weeks).
- Symptoms: Miscarriages can present with symptoms such as vaginal bleeding (which may range from light spotting to heavy bleeding), abdominal pain or cramping, and passage of tissue or clot-like material from the vagina.
- Emotional Impact: Recurrent miscarriage can have a significant emotional toll on individuals and couples, leading to feelings of grief, sadness, anxiety, and sometimes depression. Support from healthcare providers, counselors, and support groups can be crucial during this time.
- Underlying Causes: Investigating potential underlying causes is an important part of managing recurrent miscarriage. These causes may include genetic factors (chromosomal abnormalities), anatomical factors (uterine abnormalities), hormonal imbalances, autoimmune disorders, thrombophilic disorders, infections, lifestyle factors, and advanced maternal or paternal age.
COMPLICATION :
Recurrent miscarriage itself can be emotionally devastating and challenging for individuals and couples……..
- Psychological Impact: Recurrent miscarriage can lead to significant psychological distress, including feelings of grief, depression, anxiety, and loss of hope. It may also strain relationships and affect overall well-being.
- Physical Complications: While miscarriage itself is a natural process, it can sometimes lead to complications such as heavy bleeding requiring medical intervention, infection, or incomplete miscarriage (retained products of conception).
- Risk to Future Pregnancies: Each miscarriage, especially if recurrent, may increase the risk of subsequent miscarriages. Understanding and addressing underlying causes is crucial to reduce this risk.
- Impact on Fertility: Depending on the underlying cause of recurrent miscarriage, there may be implications for fertility. Addressing and treating any contributing factors can potentially improve outcomes in future pregnancies.
- Financial and Practical Considerations: Treatment for recurrent miscarriage can involve medical consultations, diagnostic tests, treatments such as hormone therapies or surgical interventions, and assisted reproductive technologies (ART). These can be costly and may require significant logistical planning.
- Underlying Health Conditions: In some cases, recurrent miscarriage may be associated with underlying health conditions such as autoimmune disorders, thrombophilic disorders, or genetic abnormalities. Identifying and managing these conditions is important for overall health.
- Long-term Emotional Consequences: Even after successful treatment and subsequent successful pregnancies, individuals and couples may experience lasting emotional effects from the trauma of recurrent miscarriage.
- Social and Support Networks: Coping with recurrent miscarriage often requires strong social support networks and access to resources such as counseling or support groups. Lack of support can exacerbate the emotional toll.
DIAGNOSTIC EVALUATION :
- Medical History: A detailed medical history is essential to understand previous pregnancies, miscarriages, any existing medical conditions (such as thyroid disorders or autoimmune diseases), medications, lifestyle factors (like smoking or substance use), and family history of reproductive issues.
- Physical Examination: A thorough physical examination may help identify any anatomical abnormalities, signs of hormonal imbalance, or other physical factors that could contribute to miscarriage.
- Blood Tests: Blood tests are typically conducted to evaluate various factors, including:
- Hormone levels (such as progesterone, thyroid hormones, androgens, and prolactin)
- Blood clotting disorders (thrombophilias)
- Antiphospholipid antibodies (which can indicate autoimmune causes)
- Immunological factors (such as autoimmune markers)
- Genetic Testing: Genetic testing may be recommended to check for chromosomal abnormalities in both partners (karyotype analysis). This can help determine if there are genetic factors contributing to recurrent miscarriage.
- Imaging Studies:
- Transvaginal Ultrasound: Used to assess the structure of the uterus and ovaries. It can identify uterine abnormalities (such as fibroids or polyps) and evaluate ovarian function.
- Hysterosalpingography (HSG): An X-ray procedure to evaluate the shape and structure of the uterus and fallopian tubes, which can detect abnormalities like uterine septum or tubal blockages.
- Hysteroscopy: A procedure where a thin, flexible tube with a camera (hysteroscope) is inserted through the cervix to examine the inside of the uterus. It can identify and potentially treat intrauterine abnormalities.
- Uterine Biopsy: In some cases, a biopsy of the uterine lining (endometrial biopsy) may be performed to assess for any chronic endometritis (inflammation of the endometrium) or other pathological conditions.
- Genetic Counseling: Genetic counseling may be recommended if genetic abnormalities are identified to discuss implications for future pregnancies and options for prenatal testing.
- Partner Evaluation: Both partners should undergo evaluation as male factors (such as sperm abnormalities or genetic factors) can also contribute to recurrent miscarriage.
- Additional Tests: Depending on specific findings and suspected causes, additional tests may be recommended. These could include testing for infections (such as TORCH infections), autoimmune disorders, or metabolic disorders.
- Specialized Testing: In some cases, specialized testing or consultation with subspecialists (such as reproductive endocrinologists or maternal-fetal medicine specialists) may be necessary for a more comprehensive evaluation.
MANAGEMENT
The management of recurrent miscarriage involves a multidisciplinary approach ……
- Identify Underlying Causes: Based on diagnostic evaluations (as mentioned earlier), the underlying causes of recurrent miscarriage will be identified. Common causes include genetic abnormalities, anatomical issues (such as uterine abnormalities), hormonal imbalances, autoimmune disorders, thrombophilic disorders, infections, and lifestyle factors.
- Treatment of Underlying Conditions:
- Genetic Abnormalities: Depending on the specific genetic findings, options such as genetic counseling, preimplantation genetic testing (PGT), or prenatal diagnosis in future pregnancies may be considered.
- Anatomical Issues: Surgical correction of uterine abnormalities (such as septum resection or removal of polyps) may be recommended to improve uterine structure and reduce the risk of miscarriage.
- Hormonal Imbalances: Hormone supplementation, particularly progesterone supplementation in early pregnancy, may be prescribed if low progesterone levels are identified.
- Autoimmune Disorders: Treatment may involve immunosuppressive therapy or other medications to manage autoimmune conditions that could potentially affect pregnancy.
- Thrombophilic Disorders: Anticoagulant therapy (blood thinners) may be prescribed to reduce the risk of blood clots that could compromise blood flow to the placenta.
- Infections: Treatment with antibiotics or antiviral medications may be necessary if infections are identified as contributing factors.
- Lifestyle Modifications: Encourage lifestyle changes that promote a healthy pregnancy, such as maintaining a balanced diet, achieving a healthy weight, avoiding smoking and excessive alcohol consumption, and managing stress.
- Supportive Care and Counseling:
- Provide emotional support and counseling to individuals and couples coping with recurrent miscarriage. This can help address grief, anxiety, and depression associated with pregnancy loss.
- Support groups or peer counseling may also be beneficial for sharing experiences and receiving support from others who have gone through similar challenges.
- Monitoring and Follow-up:
- Close monitoring during early pregnancy with frequent prenatal visits and ultrasounds to assess fetal development and address any emerging issues promptly.
- Regular follow-up appointments with healthcare providers to adjust management strategies as needed and monitor for recurrence of miscarriage risk factors.
- Assisted Reproductive Technologies (ART):
- In cases where other treatments have not been successful or if there are additional fertility issues, ART such as in vitro fertilization (IVF) with embryo testing (PGT) may be considered to improve the chances of a successful pregnancy.
- Preconception Planning:
- Optimize preconception health by addressing any modifiable risk factors before attempting to conceive again. This may include optimizing chronic medical conditions and ensuring medications are compatible with pregnancy.
- Continued Research and Evaluation:
- For cases where no specific cause is identified or where treatments are not successful, continued research and evaluation may be necessary to explore less common or emerging factors contributing to recurrent miscarriage.
PREVENTION :
Preventing recurrent miscarriage involves identifying and addressing any underlying causes that contribute to pregnancy loss. While not all cases of recurrent miscarriage can be prevented, there are several strategies that may help reduce the risk:
- Comprehensive Evaluation: Undergo a thorough diagnostic evaluation to identify potential underlying causes, such as genetic abnormalities, hormonal imbalances, anatomical issues, autoimmune disorders, thrombophilic disorders, infections, and lifestyle factors.
- Treatment of Identified Causes:
- Genetic Abnormalities: Consider genetic counseling and testing, and discuss options such as preimplantation genetic testing (PGT) or prenatal diagnosis in future pregnancies.
- Hormonal Imbalances: Address any hormonal deficiencies or imbalances through supplementation, particularly with progesterone in early pregnancy if indicated.
- Anatomical Issues: Correct any uterine abnormalities through surgical procedures such as septum resection or removal of polyps to optimize uterine environment.
- Autoimmune Disorders: Manage autoimmune conditions with appropriate medications or immunosuppressive therapy to reduce the immune response that may affect pregnancy.
- Thrombophilic Disorders: Use anticoagulant therapy (blood thinners) to prevent blood clotting disorders that could compromise blood flow to the placenta.
- Lifestyle Modifications:
- Maintain a healthy diet rich in nutrients and vitamins essential for pregnancy.
- Achieve and maintain a healthy weight.
- Avoid smoking, excessive alcohol consumption, and illicit drug use.
- Manage chronic conditions such as diabetes or hypertension under medical supervision.
- Reduce stress through relaxation techniques, counseling, or support groups.
- Preconception Planning:
- Optimize health before attempting to conceive. This includes addressing any chronic medical conditions, ensuring vaccinations are up to date, and reviewing medications with a healthcare provider to ensure they are safe for pregnancy.
- Consider consulting with a reproductive specialist or genetic counselor to discuss family planning options and potential risks.
- Regular Prenatal Care:
- Once pregnant, schedule early and regular prenatal visits to monitor the pregnancy closely.
- Follow recommendations for prenatal vitamins and supplements as advised by a healthcare provider.
- Discuss any concerns or symptoms promptly with healthcare providers to address potential complications early.
- Supportive Care:
- Seek emotional support and counseling if needed to cope with the emotional impact of recurrent miscarriage.
- Consider joining support groups or online communities to connect with others who have experienced similar challenges.
- Continued Monitoring and Adjustment:
- For individuals with recurrent miscarriage, ongoing monitoring and adjustment of management strategies may be necessary to optimize chances of a successful pregnancy.