AMENORRHEA

DEFINITION :
“Amenorrhea is the medical term for the absence of menstruation (periods).”
TYPE OF AMNORRHEA :
It can be classified into two types:
- Primary Amenorrhea: This occurs when a female has not started menstruating by the age of 16, despite having normal growth and development.
- Secondary Amenorrhea: This is the more common type and refers to the absence of menstruation for three or more consecutive months in a woman who previously had regular periods. Secondary amenorrhea can be caused by various factors, including pregnancy, hormonal imbalances, stress, excessive exercise, weight changes, and medical conditions like polycystic ovary syndrome (PCOS) or thyroid disorders.
Amenorrhea may also be a symptom of other underlying health conditions and may require medical evaluation and treatment depending on the cause.
CAUSES/ETIOLOGY :
the common causes of amenorrhea:
1. Hormonal Causes
- Hypothalamic Dysfunction: The hypothalamus regulates the release of hormones that control menstruation. Dysfunction in the hypothalamus can lead to insufficient production of gonadotropin-releasing hormone (GnRH), which results in a lack of ovulation and menstruation. This can be caused by:
- Stress: Physical or emotional stress can suppress GnRH.
- Excessive exercise: Intense physical activity can disrupt hormone balance.
- Low body weight or eating disorders (e.g., anorexia nervosa): Can lead to a decrease in body fat and hormonal disturbances.
- Pituitary Dysfunction: The pituitary gland produces hormones (FSH, LH) that stimulate the ovaries. Disorders like pituitary tumors, hypopituitarism, or Sheehan’s syndrome (damage to the pituitary after childbirth) can affect menstrual cycles.
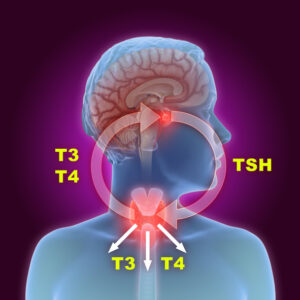
- Thyroid Disorders: Hypothyroidism (low thyroid hormone) or hyperthyroidism (excess thyroid hormone) can disrupt the menstrual cycle.
- Hyperprolactinemia: Elevated levels of prolactin, the hormone responsible for milk production, can inhibit ovulation and menstruation.
2. Ovarian Causes
- Polycystic Ovary Syndrome (PCOS): A common condition where the ovaries do not regularly release eggs, leading to hormonal imbalances and absent or irregular periods.
- Premature Ovarian Insufficiency (POI): Also known as premature menopause, this occurs when the ovaries stop functioning properly before the age of 40, leading to cessation of periods.
- Ovarian tumors or cysts: Growths or cysts on the ovaries can disrupt normal hormonal signaling, affecting menstruation.
3. Structural Causes
- Congenital Anomalies: Birth defects in the reproductive system, such as Müllerian duct abnormalities, can result in structural problems, like an absent uterus or a blocked vaginal canal, which can prevent menstruation.
- Asherman’s Syndrome: Scarring inside the uterus, often due to previous surgical procedures like curettage (D&C), can lead to amenorrhea by obstructing menstrual flow.
- Endometrial damage: Injury or damage to the lining of the uterus can also impair menstruation.
4. Pregnancy
- Pregnancy is a natural cause of secondary amenorrhea. Absence of periods is one of the most common early signs of pregnancy.
5. Medications
- Certain medications can interfere with the menstrual cycle, including:
- Hormonal contraceptives (birth control pills, IUDs, implants)
- Antipsychotic medications (can increase prolactin levels)
- Chemotherapy and radiation therapy for cancer treatment
- Antidepressants or antihypertensive medications
6. Lifestyle Factors
- Excessive exercise: Intense physical activity, especially in athletes, can lead to hormonal disruptions, causing periods to stop.
- Stress: Both emotional and physical stress can disrupt hormonal balance, leading to absent periods.
- Low body weight: Extreme weight loss, often from eating disorders or excessive physical activity, can lead to an energy imbalance that disrupts menstrual function.
7. Chronic Medical Conditions
- Diabetes: Poorly controlled diabetes can disrupt hormonal balance, leading to menstrual irregularities.
- Celiac Disease: Autoimmune disorder affecting the digestive system, which can also lead to hormonal imbalances and menstrual disturbances.
- Obesity: Excessive body fat can cause increased estrogen levels, leading to hormonal imbalances and menstrual irregularities.
8. Menopause
- Natural menopause occurs typically around age 50 and results in the permanent cessation of menstruation due to the natural decline of ovarian function.
9. Other Causes
- Excessive alcohol consumption or drug use (e.g., cocaine, marijuana) can affect hormonal levels and menstruation.
- Chronic illnesses or autoimmune disorders (such as lupus) can disrupt the endocrine system and menstruation.
CLINICAL FEATURE :
- PCOS: Irregular or absent periods, acne, excess body hair, weight gain, difficulty in conceiving.
- Hypothyroidism: Fatigue, weight gain, constipation, dry skin, cold intolerance, and absent or irregular periods.
- Hyperprolactinemia: Milky discharge from the breasts (galactorrhea), headaches, and absent periods.
- Premature Menopause: Hot flashes, night sweats, vaginal dryness, mood swings.
- Pituitary Tumors: Headaches, visual disturbances, galactorrhea, absent periods.
COMPLICATION :
Here are some of the potential complications associated with amenorrhea:
1. Infertility
- Ovulation Problems: In many cases of amenorrhea, particularly PCOS or hypothalamic dysfunction, the absence of menstruation is due to lack of ovulation. Without ovulation, a woman cannot conceive naturally.
- Premature Ovarian Insufficiency (POI): Women with early ovarian failure may experience a reduced ovarian reserve and face difficulty in getting pregnant.
- Endometrial Atrophy: Chronic absence of periods can cause the endometrial lining of the uterus to become thin and less receptive to implantation, making pregnancy less likely even if ovulation is restored later.
2. Osteoporosis (Bone Loss)
- Estrogen Deficiency: Estrogen is crucial for maintaining bone density. In cases of hypothalamic amenorrhea, PCOS, or premature ovarian insufficiency, where estrogen levels are low or absent for extended periods, women may be at increased risk for osteoporosis. This condition weakens bones, making them more susceptible to fractures.
- Long-term Amenorrhea: The longer the period of amenorrhea, the higher the risk of developing osteoporosis and fractures, especially if it is due to conditions like anorexia nervosa, where bone health is compromised.
3. Cardiovascular Risk
- Estrogen Deficiency: Estrogen has a protective effect on the cardiovascular system by regulating cholesterol levels and maintaining blood vessel health. Low estrogen levels, such as those seen in premature ovarian insufficiency or hypothalamic amenorrhea, may increase the risk of cardiovascular diseases such as heart disease, stroke, and high blood pressure.
- Metabolic Changes: Conditions like PCOS, which can cause menstrual irregularities, are also associated with an increased risk of metabolic syndrome, which includes high blood sugar, high cholesterol, and insulin resistance—all risk factors for heart disease.
4. Psychological and Emotional Impact
- Infertility Stress: Women experiencing amenorrhea due to conditions like PCOS or premature ovarian failure may struggle with infertility, which can cause significant emotional distress, anxiety, and depression.
- Body Image Issues: Conditions like anorexia nervosa or extreme exercise leading to hypothalamic amenorrhea may cause issues related to body image and self-esteem, further contributing to mental health challenges.
- Stress and Anxiety: Hormonal imbalances related to amenorrhea (e.g., hyperprolactinemia) can also cause psychological symptoms like mood swings, anxiety, and depression.
5. Endometrial Hyperplasia and Cancer
- Unopposed Estrogen: In some cases of amenorrhea (especially anovulatory cycles in PCOS or when periods are absent for extended periods), there may be high levels of estrogen without the balancing effect of progesterone. This can cause the endometrial lining to become excessively thick (endometrial hyperplasia), which increases the risk of developing endometrial cancer over time.
- Lack of Regular Bleeding: The absence of periods means that the lining of the uterus is not regularly shed, increasing the potential for abnormal cell growth in the uterus.
6. Increased Risk of Miscarriage
- Anovulation: Women with conditions such as PCOS or those who have hypothalamic amenorrhea may have difficulty ovulating regularly. This can lead to infertility, and if pregnancy does occur, there may be a higher risk of miscarriage due to hormonal imbalances that prevent proper implantation or fetal development.
7. Delayed Puberty and Growth Issues
- Primary Amenorrhea: If a girl does not begin menstruating by the age of 16, there may be an underlying issue with growth or hormonal development. This can lead to delayed puberty, affecting physical and emotional maturation, as well as affecting bone growth and overall health.
- Short Stature: In cases of hormonal imbalances that affect puberty, such as Turner syndrome, growth may be delayed, leading to short stature.
8. Increased Risk of Other Endocrine Disorders
- Thyroid Dysfunction: Women with amenorrhea due to thyroid disorders (either hypothyroidism or hyperthyroidism) may have complications related to thyroid imbalances, including weight changes, fatigue, and metabolic dysfunction. Untreated thyroid disorders can lead to more serious health issues like heart problems, fertility issues, and osteoporosis.
9. Chronic Health Conditions
- Celiac Disease or autoimmune disorders that cause secondary amenorrhea can also lead to chronic complications, including digestive problems, malabsorption of nutrients, and other organ dysfunction.
10. Vaginal and Uterine Atrophy
- Lack of Estrogen: Chronic estrogen deficiency due to long-term amenorrhea (such as in premature ovarian failure) can lead to vaginal dryness, discomfort during intercourse, and thinning of the vaginal and uterine tissues. This can also increase the risk of urinary tract infections (UTIs) and pelvic floor issues.
MANAGEMENT :
Here’s an overview of the management approach for amenorrhea:
1. Primary Amenorrhea (Failure to Menstruate by Age 16)
- Evaluation: The first step in management is to identify any underlying causes through a comprehensive assessment, including a physical examination, family history, and laboratory tests (e.g., hormone levels, karyotype analysis, imaging studies).
- Possible Treatments:
- Hormone Replacement Therapy (HRT): If the cause is related to a lack of puberty due to hormonal insufficiency (e.g., gonadal dysgenesis), treatment with estrogen and progesterone can help initiate menstrual cycles and promote the development of secondary sexual characteristics (e.g., breast development, pubic hair).
- Surgical Treatment: If there is a structural abnormality (e.g., Müllerian agenesis, or imperforate hymen), surgical intervention may be necessary to correct the anatomical issue.
- Growth Hormone Therapy: For those with growth hormone deficiency (e.g., Turner syndrome), growth hormone may be given to help promote growth and development.
2. Secondary Amenorrhea (Absence of Menstruation for 3 or More Months)
The management of secondary amenorrhea involves identifying and addressing the underlying cause. Treatment is tailored based on the diagnosis.
A. Hormonal Imbalances
- Hypothalamic Amenorrhea: Often caused by stress, excessive exercise, or low body weight.
- Lifestyle Modifications: The first line of treatment is to address contributing factors such as weight restoration, stress management, or a reduction in excessive exercise.
- Hormone Therapy: If menstruation does not resume after lifestyle changes, estrogen therapy may be prescribed to restore menstrual cycles and prevent bone loss. This can be given as oral contraceptives (birth control pills) or hormonal replacement therapy.
- Polycystic Ovary Syndrome (PCOS): A common cause of secondary amenorrhea due to anovulation (lack of ovulation).
- Oral Contraceptives: To regulate menstrual cycles, reduce androgen levels (which may cause acne or excessive hair growth), and protect against endometrial hyperplasia.
- Progestin Therapy: For women who do not wish to conceive, a progestin-only pill or IUD may be used to induce menstruation.
- Metformin: Can help improve insulin sensitivity and regulate menstrual cycles in women with insulin resistance.
- Fertility Treatment: For women seeking pregnancy, medications like clomiphene citrate or letrozole may be prescribed to induce ovulation.
- Hyperprolactinemia (Elevated Prolactin):
- Dopamine Agonists: Medications like cabergoline or bromocriptine are used to lower prolactin levels and restore menstrual cycles.
- Thyroid Dysfunction (Hypothyroidism or Hyperthyroidism):
- Thyroid Hormone Replacement: For hypothyroidism, levothyroxine can normalize thyroid hormone levels and restore menstrual cycles.
- Antithyroid Medications or Surgery: For hyperthyroidism, medications like methimazole or propylthiouracil or radioiodine therapy may be used to control thyroid function.
B. Ovarian Causes
- Premature Ovarian Insufficiency (POI):
- Hormone Replacement Therapy (HRT): To address low estrogen levels, reduce menopausal symptoms, and protect bone health. This can include estrogen (oral, transdermal) and progesterone.
- Fertility Treatment: If pregnancy is desired, assisted reproductive techniques such as egg donation may be considered.
C. Structural Causes
- Asherman’s Syndrome (Uterine Scarring):
- Hysteroscopic Surgery: To remove scar tissue inside the uterus, allowing normal menstruation to resume.
- Müllerian Anomalies (e.g., Vaginal or Uterine Agenesis):
- Surgical correction may be necessary to create or reconstruct the vaginal canal.
- Hormone therapy may still be required for secondary sexual characteristic development.
D. Lifestyle Factors
- Stress-Induced Amenorrhea:
- Psychological Support: Counseling, stress management techniques, and lifestyle changes to reduce stress may be helpful.
- Excessive Exercise and Low Body Weight:
- Nutritional Counseling: Restoring a healthy weight and a balanced diet is crucial. Women with anorexia nervosa may require a multidisciplinary approach including medical, nutritional, and psychological support.
- Reducing Exercise Intensity: Gradual reduction of excessive physical activity is often recommended to restore normal hormonal function.
3. Fertility Treatments (if pregnancy is desired)
- Ovulation Induction: If ovulation is absent (e.g., in PCOS or hypothalamic amenorrhea), medications such as clomiphene citrate, letrozole, or gonadotropins can be used to stimulate ovulation.
- In Vitro Fertilization (IVF): In cases where other fertility treatments are unsuccessful, IVF may be considered.
4. Management of Underlying Conditions
- Celiac Disease or other autoimmune conditions may require the treatment of the primary condition (e.g., a gluten-free diet for celiac disease) to restore normal menstruation.
- Diabetes Management: Tight blood sugar control in women with diabetes is important to normalize menstrual cycles.
5. Psychological Support
- Women with anorexia nervosa, stress-induced amenorrhea, or infertility-related emotional distress may benefit from psychotherapy (cognitive-behavioral therapy) and support groups to address the emotional and psychological impact of amenorrhea.
- Cognitive Behavioral Therapy (CBT) may help with body image issues, particularly in those with eating disorders.
6. Bone Health
- Women with hypothalamic amenorrhea or premature ovarian insufficiency are at increased risk of osteoporosis due to low estrogen levels. In such cases:
- Calcium and Vitamin D supplementation is recommended.
- Bisphosphonates or denosumab may be prescribed to prevent bone loss in some cases.