CERVICAL INCOMPETENCE
DEFINITION :
” Cervical incompetence, also known as incompetent cervix or cervical insufficiency, is a condition where the cervix (the lower part of the uterus that opens into the vagina) begins to dilate and efface (thin out) prematurely, typically during the second trimester of pregnancy, leading to spontaneous miscarriage or preterm birth. Normally, the cervix remains closed and firm throughout pregnancy until it gradually softens and dilates near the time of delivery.”
INCIDENCE :
- The incidence of cervical incompetence is estimated to be relatively low, affecting about 1% to 2% of all pregnancies.
ETIOLOGY /CAUSES :
The etiology of cervical incompetence can be multifactorial and is not always fully understood. Some of the potential causes and contributing factors include:
- Congenital Factors: Some women may have a congenitally short or abnormally structured cervix that predisposes them to cervical incompetence.
- Previous Cervical Surgery: Procedures such as cone biopsy or cervical cerclage (a surgical procedure to reinforce the cervix) may weaken the cervix and increase the risk of incompetence.
- Uterine Anomalies: Certain uterine abnormalities, such as a bicornuate uterus or septate uterus, can affect cervical function and increase the risk of incompetence.
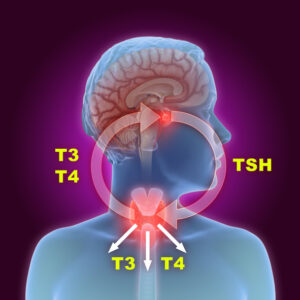
- Hormonal Influences: Imbalances in hormones such as progesterone, which helps maintain the integrity of the cervix, may contribute to cervical incompetence.
- Trauma or Injury: Trauma to the cervix from procedures, accidents, or previous difficult births may weaken the cervix and lead to incompetence.
- Infections: Certain infections, such as intrauterine infections or sexually transmitted infections, may affect cervical health and contribute to incompetence.
- Miscellaneous Factors: Other factors such as maternal age, multiple pregnancies (e.g., twins or higher-order multiples), and genetic predispositions may also play a role in cervical incompetence.
CLINICAL FEATURE :
Clinical features of cervical incompetence typically manifest as follows:
- Second-Trimester Pregnancy Loss: The most common presentation is painless dilation and effacement of the cervix leading to spontaneous miscarriage or stillbirth during the second trimester (usually between 16 to 24 weeks gestation).
- Recurrent Pregnancy Loss: Women with cervical incompetence may experience multiple consecutive miscarriages in the second trimester, often without any signs of labor or contractions.
- Shortened Cervical Length: During routine prenatal care or ultrasound examinations, a shortened cervical length (<25 mm) may be detected. This can be an indicator of cervical incompetence and increased risk of preterm birth.
- History of Previous Preterm Birth: Women with a history of preterm birth, especially due to painless cervical dilation and pregnancy loss in the second trimester, may suggest a predisposition to cervical incompetence.
- No Signs of Labor: Unlike normal labor, cervical incompetence often presents without the typical signs and symptoms of labor such as contractions or rupture of membranes. Instead, there may be painless cervical dilation and descent of the fetus.
- Cervical Examination Findings: On physical examination, the cervix may appear soft, shortened, and dilated prematurely in women with cervical incompetence, especially if evaluated during the second trimester.
COMPLICATION :
Cervical incompetence can lead to several serious complications for both the mother and the fetus:
- Pregnancy Loss: The most immediate complication of cervical incompetence is the loss of pregnancy, typically occurring in the second trimester. This can result in miscarriage or stillbirth.
- Preterm Birth: Cervical incompetence is a significant risk factor for preterm birth, where the baby is born before 37 weeks of gestation. Preterm birth can lead to a range of complications for the baby, including respiratory distress syndrome, neurological problems, and long-term developmental issues.
- Chorioamnionitis: Prolonged cervical dilation and rupture of membranes due to incompetence can increase the risk of intrauterine infection, known as chorioamnionitis. This infection can lead to maternal fever, uterine tenderness, and potentially life-threatening complications such as sepsis.
- Placental Abruption: In some cases, premature dilation of the cervix can lead to placental abruption, where the placenta separates from the uterine wall before delivery. Placental abruption can cause heavy bleeding, fetal distress, and in severe cases, can be life-threatening for both the mother and the baby.
- Postpartum Hemorrhage: After delivery, women with cervical incompetence may be at increased risk of postpartum hemorrhage due to the potential for uterine atony (lack of uterine muscle tone) and trauma associated with preterm delivery.
- Psychological Impact: Experiencing recurrent pregnancy loss or preterm birth due to cervical incompetence can have a significant emotional toll on women and their families, leading to anxiety, depression, and other psychological issues.
INVESTIGATION :
- Transvaginal Ultrasound (TVUS):
- Cervical Length Measurement: TVUS is used to measure the length of the cervix. A shortened cervical length (<25 mm) in the mid-trimester (usually between 16 to 24 weeks) is suggestive of cervical incompetence.
- Cervical Funneling: This refers to the widening of the internal os of the cervix and can be visualized on ultrasound. Funneling is a sign that the cervix may be opening prematurely.
- History and Physical Examination:
- A thorough history, including previous obstetric history (such as previous preterm births or second-trimester losses), cervical surgeries (like cone biopsy), and any known uterine anomalies, is important.
- Physical examination may reveal softening, shortening, or dilation of the cervix during speculum examination.
- Cervical Biopsy (Optional):
- In cases where there is suspicion of cervical abnormalities or if the cause is unclear, a cervical biopsy may be performed to evaluate for any structural or pathological changes.
- Laboratory Tests:
- Routine prenatal tests may be conducted to assess for infections or other conditions that could potentially affect cervical health and pregnancy outcomes.
- Serial Cervical Assessments:
- Women at high risk for cervical incompetence may undergo serial cervical assessments via TVUS to monitor cervical length and changes over time during pregnancy.
- Other Imaging Modalities:
- In some cases, additional imaging such as magnetic resonance imaging (MRI) or hysterosalpingography (HSG) may be used to evaluate uterine anatomy and confirm or rule out structural abnormalities contributing to cervical incompetence.
- Genetic Counseling and Testing:
- Genetic counseling and testing may be considered if there are concerns about underlying genetic factors contributing to cervical incompetence, particularly in cases of recurrent losses or familial history.
MANAGEMENT :
Here are the main strategies used in the management of cervical incompetence:
- Cervical Cerclage:
- Transvaginal Cerclage: This is a surgical procedure where a stitch (suture) is placed around the cervix to reinforce and support it. It is typically performed prophylactically (electively) in women with a history of cervical incompetence or short cervix detected in mid-trimester ultrasound.
- Emergency Cerclage: In cases where cervical incompetence is suspected or diagnosed after cervical dilation has begun without contractions, an emergency cerclage may be considered to attempt to halt further cervical changes and prolong the pregnancy.
- Progesterone Supplementation:
- Progesterone, a hormone that helps maintain the uterine lining and pregnancy, may be prescribed to women at risk of cervical incompetence, particularly if there is a history of preterm birth. It can help reduce the risk of preterm labor and birth.
- Cervical Pessary:
- A cervical pessary is a silicone device placed around the cervix to provide mechanical support. It may be considered as an alternative to cerclage in some cases, although its effectiveness is still under investigation and it is not universally used.
- Monitoring and Serial Cervical Assessments:
- Regular monitoring of cervical length via transvaginal ultrasound throughout pregnancy helps to detect early signs of cervical changes and allows for timely intervention if necessary.
- Bed Rest and Activity Restrictions:
- In some cases, modified activity or bed rest may be recommended to reduce pressure on the cervix and minimize the risk of cervical changes.
- Antibiotics:
- Antibiotics may be prescribed if there is evidence of infection or to prevent infection following cervical procedures such as cerclage.
- Patient Education and Counseling:
- Providing education on signs and symptoms of preterm labor, encouraging regular prenatal care visits, and addressing any concerns or questions the patient may have are important aspects of management.
- Psychological Support:
- Given the emotional stress associated with cervical incompetence and its potential consequences, offering psychological support and counseling to patients and their families is crucial.
PREVENTION :
Preventing cervical incompetence focuses on identifying and managing risk factors that contribute to the condition.
- Preconception Counseling:
- Women with a history of cervical surgery, such as cone biopsy, should receive preconception counseling. Discussing the potential risks of cervical incompetence and strategies for prevention, such as cervical cerclage, can be beneficial.
- Screening and Monitoring:
- Routine prenatal care should include screening for cervical length via transvaginal ultrasound, especially in women with risk factors or a history of preterm birth. Early detection of a short cervix allows for timely intervention.
- Cervical Cerclage:
- Prophylactic cervical cerclage may be considered in women with a history of cervical incompetence or previous second-trimester pregnancy loss due to cervical dilation. This preventive measure is typically performed around 12-14 weeks of gestation.
- Progesterone Supplementation:
- Progesterone supplementation may be recommended for women at high risk of preterm birth, including those with a history of preterm delivery. This hormone helps maintain the uterine environment and may reduce the risk of cervical changes leading to incompetence.
- Avoiding Risk Factors:
- Minimizing exposure to factors that can weaken the cervix, such as avoiding excessive physical strain or trauma to the cervix, may help reduce the risk of cervical incompetence.
- Managing Infections:
- Prompt treatment of infections that can affect cervical health, such as sexually transmitted infections or intrauterine infections, is important. Regular screening and appropriate management of infections can help prevent complications that contribute to cervical incompetence.
- Lifestyle Modifications:
- Maintaining a healthy lifestyle, including a balanced diet, regular exercise (as recommended by healthcare providers), and avoiding smoking and alcohol consumption, can contribute to overall maternal health and potentially reduce the risk of cervical incompetence.
- Genetic Counseling:
- In cases where there is a suspected genetic component to cervical incompetence, genetic counseling may be beneficial. Understanding genetic risks can help in making informed decisions about family planning and pregnancy management.