ECTOPIC PREGNANCY
Here are some key points regarding the incidence of ectopic pregnancy:
- Overall Incidence: Ectopic pregnancy occurs in approximately 1-2% of all pregnancies.
- Trends: The incidence of ectopic pregnancy has been relatively stable over the years in many developed countries, though specific trends may vary. In the United States, for example, there were about 19.7 ectopic pregnancies per 1,000 live births in 2017.
- Geographic Variation: Rates of ectopic pregnancy can vary significantly between different regions and countries. Factors such as access to healthcare, prevalence of sexually transmitted infections, and contraceptive practices can influence these variations.
The etiology of ectopic pregnancy involves several factors that contribute to the implantation of the fertilized egg outside the uterus, typically in the fallopian tubes……
- Fallopian Tube Abnormalities: Any condition that affects the structure or function of the fallopian tubes can increase the risk of ectopic pregnancy. This includes previous surgery on the tubes, such as tubal ligation or tubal reconstruction, as well as congenital abnormalities.
- Pelvic Inflammatory Disease (PID): Infections of the reproductive organs, often caused by sexually transmitted infections (STIs) such as chlamydia or gonorrhea, can lead to scarring and narrowing of the fallopian tubes. This scarring can prevent the fertilized egg from reaching the uterus, resulting in implantation in the fallopian tube.
- Previous Ectopic Pregnancy: Women who have had an ectopic pregnancy in the past are at a higher risk of experiencing another one in subsequent pregnancies.
- Endometriosis: This condition can cause the growth of endometrial-like tissue outside the uterus, including in the fallopian tubes. This can interfere with the movement of the fertilized egg and increase the likelihood of ectopic pregnancy.
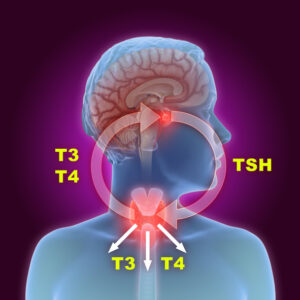
- Hormonal Factors: Abnormal levels of certain hormones, such as progesterone, can affect the ability of the fertilized egg to implant properly within the uterus, leading to ectopic implantation.
- Smoking: Tobacco use has been linked to an increased risk of ectopic pregnancy, possibly due to its effects on the fallopian tubes and hormonal balance.
- Assisted Reproductive Techniques: Procedures such as in vitro fertilization (IVF) can increase the likelihood of ectopic pregnancy, primarily because the process bypasses natural fallopian tube transport of the embryo, increasing the chances of implantation outside the uterus.
- IUD Use: While rare, intrauterine devices (IUDs) can fail to prevent pregnancy and when pregnancy occurs, there’s a slightly higher risk of it being ectopic.
RISK FACTOR :
Here are some key risk factors:
- Previous Ectopic Pregnancy: Women who have had an ectopic pregnancy before are at a higher risk of experiencing another one in subsequent pregnancies.
- Pelvic Inflammatory Disease (PID): Infections of the reproductive organs, often caused by sexually transmitted infections (STIs) such as chlamydia or gonorrhea, can lead to scarring and narrowing of the fallopian tubes. This scarring can increase the risk of an ectopic pregnancy.
- Pelvic Surgery: Previous surgery on the fallopian tubes or pelvic area, such as surgery to treat an ectopic pregnancy or to reverse a tubal ligation, can increase the risk of ectopic pregnancy due to scarring or damage to the fallopian tubes.
- Inflammation or Endometriosis: Conditions that cause inflammation in the pelvic area or abnormal growth of tissue, such as endometriosis, can disrupt the normal function and structure of the fallopian tubes, increasing the risk of ectopic pregnancy.
- Use of Assisted Reproductive Technology (ART): Procedures such as in vitro fertilization (IVF) can increase the risk of ectopic pregnancy because the fertilized embryo is transferred directly into the uterus or fallopian tubes, bypassing natural mechanisms that help ensure proper implantation in the uterus.
- Smoking: Tobacco use has been associated with an increased risk of ectopic pregnancy, likely due to its effect on the fallopian tubes and hormonal balance.
- Age: While ectopic pregnancy can occur at any age during the reproductive years, the risk may be slightly higher in women over 35.
- Contraceptive Use: While rare, pregnancies can occur with intrauterine devices (IUDs) in place, and if pregnancy does happen, there is a slightly higher risk that it may be ectopic.
- Tubal Surgery or Abnormalities: Any surgery on the fallopian tubes or congenital abnormalities of the tubes can increase the likelihood of ectopic pregnancy.
- Progestin-only Contraceptives: There is a slight increase in risk with progestin-only contraceptives like the mini-pill, though the overall risk remains low compared to no contraception.
SITE OF IMPLANTATION IN ECTOPIC PREGNANCY :
In ectopic pregnancy, the fertilized egg implants outside the uterine cavity, typically in one of the following locations:
- Fallopian Tubes: This is the most common site of implantation in ectopic pregnancies, accounting for approximately 95% of cases. Within the fallopian tubes, implantation can occur in different segments:
- Ampullary: The widest part of the fallopian tube, just before it meets the uterus.
- Isthmic: The narrower portion of the fallopian tube closer to the uterus.
- Interstitial: Also known as cornual pregnancy, where the embryo implants in the proximal part of the fallopian tube that penetrates the uterine wall.
- Ovaries: Ectopic pregnancies can also implant on the surface of the ovary. This is less common than tubal ectopic pregnancies but can occur.
- Abdominal Cavity: In rare cases, the fertilized egg may implant within the abdominal cavity, often on organs such as the abdominal wall, intestines, or liver. This is known as an abdominal ectopic pregnancy.
- Cervix: Although very rare, ectopic pregnancies can implant in the cervix, the lower part of the uterus that connects to the vagina.
- Heterotopic Pregnancy: In some extremely rare instances, particularly in pregnancies resulting from assisted reproductive technologies (such as IVF), there can be both an ectopic pregnancy (typically in the fallopian tube) and an intrauterine pregnancy occurring simultaneously. This is known as a heterotopic pregnancy.
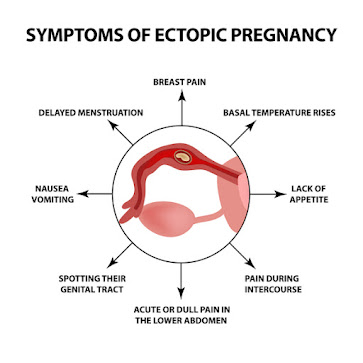
CLINICAL FEATURE :
The clinical features of ectopic pregnancy can vary depending on the location of implantation and the stage of pregnancy. Here are the typical clinical features:
- Abdominal or Pelvic Pain: This is the most common symptom of ectopic pregnancy. The pain is often sharp and may be localized on one side of the lower abdomen or pelvis. It can range from mild discomfort to severe, intense pain.
- Vaginal Bleeding: Light vaginal bleeding or spotting can occur in ectopic pregnancy. This bleeding may be lighter or heavier than a normal menstrual period and may be accompanied by abdominal pain.
- Missed Menstrual Period: Some women with ectopic pregnancy may initially experience a missed period, which can lead to suspicion of pregnancy. However, subsequent symptoms such as pain and bleeding may indicate an ectopic pregnancy rather than a normal intrauterine pregnancy.
- Shoulder Tip Pain: This specific type of pain occurs due to irritation of the diaphragm by blood or fluid from a ruptured ectopic pregnancy. It is a referred pain felt in the shoulder area and can be a sign of significant internal bleeding.
- Signs of Shock: In cases of ruptured ectopic pregnancy with severe internal bleeding, symptoms of shock may develop, including dizziness, fainting, rapid pulse, and low blood pressure.
- Gastrointestinal Symptoms: Nausea, vomiting, diarrhea, or abdominal bloating may occur, which can mimic symptoms of other gastrointestinal conditions.
- Positive Pregnancy Test: A positive pregnancy test is usually present in ectopic pregnancy because the body produces the pregnancy hormone hCG (human chorionic gonadotropin). However, hCG levels may rise more slowly or plateau compared to a normal intrauterine pregnancy.
- Adnexal Mass: On physical examination, a mass or tenderness may be felt in the pelvic area, especially near the affected fallopian tube.
COMPLICATION :
- Tubal Rupture: This is the most severe complication of ectopic pregnancy. As the embryo grows in the fallopian tube, it can cause the tube to stretch and eventually rupture. This can lead to severe abdominal pain, internal bleeding, and potentially life-threatening hemorrhage. Prompt surgical intervention is required to manage a ruptured ectopic pregnancy.
- Hemorrhage: Even before rupture, an ectopic pregnancy can cause significant internal bleeding due to the growing embryo disrupting blood vessels within the fallopian tube or surrounding tissues. This bleeding can lead to symptoms such as dizziness, fainting, and signs of shock.
- Pelvic Infection: An ectopic pregnancy can increase the risk of pelvic inflammatory disease (PID), especially if there is a delay in diagnosis or treatment. PID can cause fever, pelvic pain, and may require antibiotic treatment.
- Infertility: Depending on the extent of damage to the fallopian tubes, ectopic pregnancy and its treatment (such as surgical removal of the affected tube) can impact future fertility. If both fallopian tubes are affected, fertility may be significantly impaired.
- Psychological Impact: Dealing with the emotional and psychological impact of an ectopic pregnancy, especially if it results in loss of pregnancy or complications, can be challenging for individuals and their partners.
- Repeat Ectopic Pregnancy: Women who have had one ectopic pregnancy are at increased risk of having another in future pregnancies. Proper monitoring and management are essential for subsequent pregnancies.
- Medical and Surgical Complications: Depending on the treatment approach (medical management with methotrexate or surgical intervention), there can be risks of adverse effects from medications or complications related to surgery.
INVESTIGATION IN ECTOPIC PREGNANCY :
Here are the main investigations commonly used in the evaluation of ectopic pregnancy:
- Pregnancy Test:
- A urine or blood pregnancy test is typically the first step to confirm pregnancy. In ectopic pregnancy, the test will be positive because the body produces the pregnancy hormone hCG (human chorionic gonadotropin). Serial hCG measurements over time can provide important information about the progression of the pregnancy.
- Transvaginal Ultrasound:
- Transvaginal ultrasound is the primary imaging modality used to diagnose ectopic pregnancy and determine its location.
- Gestational Sac: In ectopic pregnancy, the gestational sac may be visualized outside the uterine cavity. The most common location is within the fallopian tubes (tubal ectopic pregnancy).
- Empty Uterus: In cases of ectopic pregnancy, the uterus may appear empty or smaller than expected for the gestational age if there is no intrauterine pregnancy.
- Presence of Fetal Heartbeat: In cases where the ectopic pregnancy is advanced or in cases of heterotopic pregnancy (where both ectopic and intrauterine pregnancies coexist), the presence or absence of a fetal heartbeat may be assessed.
- Serum hCG Levels:
- Serial measurement of serum hCG levels is essential in the evaluation of ectopic pregnancy. In a normal pregnancy, hCG levels typically double every 48-72 hours during the early weeks of pregnancy. In ectopic pregnancy, the rate of rise may be slower or plateau.
- Comparing ultrasound findings with hCG levels helps confirm the diagnosis and monitor treatment response.
- Additional Imaging:
- Abdominal Ultrasound: If transvaginal ultrasound is inconclusive or additional information is needed, abdominal ultrasound may be performed to assess the pelvic and abdominal organs.
- MRI: Magnetic Resonance Imaging (MRI) can provide detailed imaging of pelvic structures and may be used in cases where ultrasound findings are unclear or to evaluate for suspected complications such as rupture.
- Culdocentesis:
- Culdocentesis involves inserting a needle into the cul-de-sac (space behind the uterus) to detect the presence of blood. It may be used in cases of suspected rupture of an ectopic pregnancy.
- Laparoscopy or Laparotomy:
- If there is diagnostic uncertainty, suspicion of a complex ectopic pregnancy (e.g., heterotopic pregnancy), or if surgical intervention is planned, laparoscopy (minimally invasive surgery) or laparotomy (open surgery) may be performed for direct visualization and treatment.
- Clinical Assessment:
- A thorough clinical assessment including history taking (e.g., risk factors for ectopic pregnancy), physical examination (e.g., pelvic tenderness or mass), and evaluation of vital signs (e.g., signs of shock in cases of rupture) is crucial in the evaluation of ectopic pregnancy.
MANAGEMENT :
- Expectant Management: In cases where the ectopic pregnancy is small, stable, and hCG levels are low, expectant management (watchful waiting) may be an option. This involves monitoring the woman closely with serial hCG levels and ultrasound scans to ensure the ectopic pregnancy resolves on its own without intervention. This approach is typically considered only in very early ectopic pregnancies and when there are no signs of complications.
- Medical Management: The most common medication used for medical management of ectopic pregnancy is methotrexate. Methotrexate is a folic acid antagonist that stops the growth of rapidly dividing cells, including the trophoblast cells of the ectopic pregnancy. It is typically administered as a single or sometimes multiple doses, and it allows the body to reabsorb the ectopic pregnancy over time. Candidates for methotrexate treatment must meet specific criteria including stable vital signs, low and declining hCG levels, and absence of fetal cardiac activity.
- Surgical Management:
- Laparoscopic Surgery: This is the preferred surgical approach for ectopic pregnancy in many cases. It involves making small incisions in the abdomen to access and remove the ectopic pregnancy while preserving the affected fallopian tube whenever possible. Laparoscopic surgery is associated with faster recovery times compared to open abdominal surgery.
- Laparotomy: In cases where the ectopic pregnancy has ruptured or is large, open abdominal surgery (laparotomy) may be necessary. This involves a larger incision in the abdomen to remove the ectopic pregnancy and manage any bleeding or damage to nearby organs.
- Follow-up: After treatment, follow-up care is essential to monitor recovery, assess hCG levels to ensure they return to non-pregnant levels, and to check for any complications or recurrence. Counseling regarding future fertility and contraception options may also be provided.
- Emergency Management: If a ruptured ectopic pregnancy causes severe bleeding and shock, emergency medical attention is required. This may involve immediate surgical intervention to stop bleeding and stabilize the woman’s condition.
PREVENTION :
Here are several strategies and considerations for preventing ectopic pregnancy:
- Sexual Health Education: Educating individuals about sexually transmitted infections (STIs) and promoting safe sex practices can help reduce the risk of pelvic inflammatory disease (PID), which is a major risk factor for ectopic pregnancy.
- STI Screening and Treatment: Routine screening for STIs and prompt treatment of infections can help prevent PID and reduce the risk of fallopian tube damage that can lead to ectopic pregnancy.
- Contraception: Effective contraception can help prevent unintended pregnancies, including ectopic pregnancies. Options such as barrier methods (condoms), hormonal contraceptives (pills, patches, injections), and intrauterine devices (IUDs) can all help reduce the risk of pregnancy when used consistently and correctly.
- Early Detection and Management of Pregnancy: Early detection and confirmation of pregnancy through regular pregnancy testing can help ensure timely medical evaluation. This is important because early diagnosis of ectopic pregnancy allows for early intervention and management, which can reduce complications.
- Prompt Medical Evaluation: Women who experience symptoms such as abdominal pain, vaginal bleeding, or other unusual symptoms should seek prompt medical evaluation. Early diagnosis of ectopic pregnancy can prevent complications such as tubal rupture and severe bleeding.
- Monitoring High-Risk Groups: Women who are at increased risk of ectopic pregnancy (such as those with a history of PID, previous ectopic pregnancy, or tubal surgery) may benefit from closer monitoring and early pregnancy testing to detect ectopic pregnancy as soon as possible.
- Assisted Reproductive Technologies (ART): For women undergoing fertility treatments such as in vitro fertilization (IVF), strategies to minimize the risk of ectopic pregnancy include careful monitoring of ovarian response, embryo quality, and proper placement during embryo transfer.
- Counseling and Support: Providing education and counseling about ectopic pregnancy risk factors, symptoms, and the importance of early medical consultation can empower individuals to seek timely care when needed.