INCOMPLETE MISCARRIAGE
DEFINITION :
” When the entire product of conception are not expelled , instead a part of it is left inside the uterine cavity , is called incomplete miscarriage “
INCIDENCE :
- Generally, the reported incidence of incomplete miscarriage ranges from about 10% to 25% of all miscarriages.
ETIOLOGY / CAUSES :
Incomplete miscarriage can occur due to various factors, both maternal and fetal. Here are some of the common causes or etiological factors that contribute to incomplete miscarriage:
- Retained Products of Conception (POC): This is the most common cause of incomplete miscarriage. It happens when not all fetal tissue, placenta, or products of conception are expelled from the uterus after a miscarriage. This can lead to persistent bleeding, cramping, and potential infection if not managed promptly.
- Uterine Abnormalities: Structural issues with the uterus, such as fibroids (benign growths), uterine septum (a wall or partition within the uterus), or congenital anomalies, can contribute to incomplete miscarriage by preventing complete expulsion of fetal tissue.
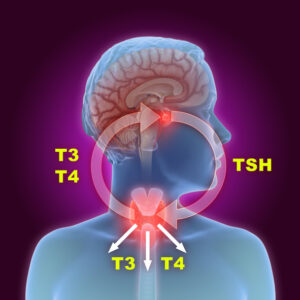
- Hormonal Imbalances: Hormonal factors, such as insufficient production of progesterone (which supports the uterine lining during pregnancy), can contribute to miscarriage and potentially incomplete expulsion of uterine contents.
- Maternal Age: Advanced maternal age is associated with an increased risk of miscarriage due to chromosomal abnormalities in the embryo, which can also contribute to incomplete miscarriage.
- Infections: Infections of the uterus or reproductive organs can interfere with the natural process of miscarriage and lead to incomplete expulsion of fetal tissue.
- Medical Conditions: Certain maternal medical conditions, such as diabetes, thyroid disorders, autoimmune diseases, or clotting disorders, can increase the risk of miscarriage and potentially incomplete miscarriage.
- Trauma or Injury: Physical trauma or injury to the abdomen or uterus can disrupt the normal process of miscarriage and lead to incomplete expulsion of fetal tissue.
- Environmental Factors: Exposure to environmental toxins, radiation, certain medications, or recreational drugs may also contribute to miscarriage and potentially incomplete miscarriage.
- Genetic Factors: In some cases, genetic abnormalities in the embryo or fetus can lead to miscarriage and incomplete expulsion of fetal tissue.
CLINICAL FEATURE :
Incomplete miscarriage presents with several clinical features that help clinicians diagnose and manage the condition. These features include:
- Vaginal Bleeding: This is often the first and most prominent symptom. Bleeding can range from light spotting to heavy bleeding and may be accompanied by passage of clots or tissue.
- Cramping: Women with incomplete miscarriage typically experience abdominal cramping or pain, which can range from mild to severe. The pain is often associated with the process of uterine contraction to expel remaining tissue.
- Passage of Tissue: Patients may pass clots or tissue from the vagina. This tissue may appear grayish or pinkish and may be identified as fetal tissue or placental remnants.
- Persistent Pregnancy Symptoms: Some women may continue to experience symptoms of pregnancy, such as breast tenderness, nausea, or fatigue, even after a miscarriage has begun.
- Fever or Chills: In cases where there is infection or retained tissue leading to infection, fever and chills may develop as signs of systemic involvement.
- Incomplete Emptying of the Uterus: On clinical examination, the uterus may feel larger than expected for the gestational age or may still contain palpable tissue or clots.
- Pain or Tenderness on Pelvic Examination: Pelvic examination may reveal tenderness or pain upon palpation of the uterus or adnexal regions.
- Ultrasound Findings: Transvaginal ultrasound is often used to confirm the diagnosis of incomplete miscarriage. It may show retained products of conception within the uterus, thickened endometrium, or other signs suggestive of incomplete evacuation.
- Uterus is smaller than period of amenorrhea
COMPLICATION :
Incomplete miscarriage can lead to several complications if not properly managed. Some of the potential complications include:
- Excessive Bleeding: Retained products of conception can cause ongoing or heavy bleeding from the uterus. This can lead to significant blood loss (hemorrhage), which may require medical intervention to control.
- Infection: When fetal or placental tissue remains in the uterus, it can serve as a focus for infection. This can lead to endometritis (infection of the uterine lining) or pelvic inflammatory disease (PID), which can cause fever, chills, abdominal pain, and potentially serious systemic infection.
- Anemia: Prolonged or heavy bleeding associated with incomplete miscarriage can lead to iron deficiency anemia due to blood loss over time.
- Future Fertility Issues: In some cases, incomplete miscarriage or the complications thereof (such as infection or uterine scarring from surgical procedures) can affect future fertility by compromising the normal function of the uterus or fallopian tubes.
- Psychological Impact: Miscarriage, especially when complicated by incomplete miscarriage or medical interventions, can have a profound emotional impact on individuals and their partners. Feelings of grief, sadness, anxiety, or guilt are common and may require emotional support or counseling.
- Retained Tissue or Persistent Symptoms: Incomplete miscarriage may necessitate additional medical procedures, such as repeated doses of medications or a second surgical intervention (repeat D&C), if initial management does not fully resolve the condition.
- Septicemia: In rare cases, severe infection from retained products of conception can lead to septicemia, a life-threatening systemic infection that requires urgent medical treatment.