OLIGOMENORRHEA

DEFINITION :
“Oligomenorrhea is a medical term used to describe infrequent or irregular menstrual periods.”
ETIOLOGY/CAUSES :
The etiology (causes) of oligomenorrhea can be multifactorial, and it often arises due to disruptions in the hormonal regulation of the menstrual cycle. Some common causes include:
1. Hormonal Imbalances
- Polycystic Ovary Syndrome (PCOS): A common condition where hormonal imbalances lead to irregular or infrequent periods due to the presence of cysts on the ovaries.
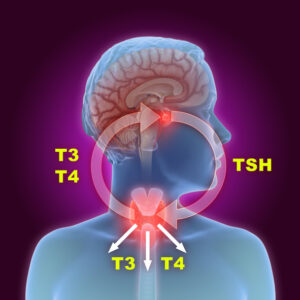
- Hypothyroidism: Underactive thyroid function can interfere with the regularity of the menstrual cycle.
- Hyperprolactinemia: High levels of prolactin (a hormone produced by the pituitary gland) can suppress ovulation and menstrual bleeding.
- Luteal phase defects: Problems with the second half of the menstrual cycle (the luteal phase) can cause irregularities in the menstrual cycle.
- Premature Ovarian Insufficiency (POI): When the ovaries stop functioning properly before the age of 40, leading to irregular periods or cessation of menstruation.
2. Stress and Emotional Factors
- Physical or emotional stress can disrupt the hypothalamus, which controls the pituitary gland and regulates the menstrual cycle, leading to irregular periods.
- Eating disorders (e.g., anorexia or bulimia) can also cause stress to the body, leading to hormonal imbalances and oligomenorrhea.
3. Excessive Exercise or Low Body Weight
- Athletic Amenorrhea: Intense physical activity, especially combined with low body fat, can disrupt hormonal balance, causing infrequent periods.
- Severe Weight Loss or Underweight: Drastic weight loss can lead to a decrease in estrogen levels, which may result in irregular or absent periods.
4. Obesity
- Excessive body fat can lead to increased levels of estrogen, which may interfere with ovulation and cause irregular menstrual cycles.
5. Medications
- Certain medications, such as birth control pills, antipsychotics, or chemotherapy drugs, can affect the menstrual cycle, leading to oligomenorrhea.
6. Chronic Medical Conditions
- Diabetes: Poorly controlled diabetes can lead to hormonal imbalances affecting the menstrual cycle.
- Cushing’s Syndrome: High levels of cortisol due to a disorder of the adrenal glands can cause menstrual irregularities.
- Hyperandrogenism: Elevated levels of male hormones (androgens) can lead to infrequent menstruation, often seen in PCOS.
7. Perimenopause
- As women approach menopause, their hormone levels fluctuate, which may lead to irregular periods, including oligomenorrhea.
8. Genetic Factors
- Some women may have a genetic predisposition to irregular menstrual cycles or conditions such as PCOS.
CLINICAL FEATURE :
characteristics and associated symptoms:
1. Infrequent Menstrual Periods
- The hallmark of oligomenorrhea is menstrual cycles that occur more than 35 days apart but less than 6 months apart, typically fewer than 9 periods per year.
2. Irregular Cycle Length
- Women with oligomenorrhea may experience highly variable cycle lengths, meaning their periods do not follow a predictable pattern.
3. Absence of Ovulation (Anovulation)
- Oligomenorrhea often accompanies anovulation, where the ovaries do not release an egg during the cycle. This can result in difficulty conceiving, as ovulation is necessary for pregnancy.
4. Infertility
- Since ovulation is often irregular or absent, fertility problems may arise, and women may experience difficulty getting pregnant.
5. Acne and Hirsutism
- If oligomenorrhea is related to conditions like polycystic ovary syndrome (PCOS), women may also experience symptoms like excessive facial or body hair (hirsutism) and acne due to elevated levels of androgens (male hormones).
6. Weight Changes
- Women with oligomenorrhea may experience weight gain or difficulty losing weight, particularly if the condition is linked to hormonal imbalances, such as in PCOS or thyroid disorders.
7. Pelvic Pain or Discomfort
- Some women with oligomenorrhea, particularly those with PCOS or other reproductive disorders, may experience chronic pelvic pain or painful periods when menstruation does occur.
8. Hair Thinning
- In some cases, women may experience thinning hair or hair loss, particularly if the condition is associated with an excess of androgens.
9. Fatigue
- Some women report feeling fatigued or having low energy, which can be a side effect of hormonal imbalances or conditions like thyroid dysfunction or PCOS.
10. Mood Swings or Depression
- Hormonal imbalances associated with oligomenorrhea can lead to mood changes, such as irritability or symptoms of depression and anxiety.
11. Signs of Underlying Conditions
- If oligomenorrhea is linked to other medical conditions, such as hypothyroidism or Cushing’s syndrome, the woman may show additional symptoms specific to those disorders, such as dry skin or weight gain (in hypothyroidism) or excessive hair growth and round face (in Cushing’s syndrome).
12. No Menstrual Bleeding (Amenorrhea)
- In some severe cases, oligomenorrhea can progress to amenorrhea, the complete absence of menstruation for more than 3 months, especially if the underlying cause is related to conditions like premature ovarian failure or hypothalamic dysfunction.
COMPLICATION :
Some of the main complications associated with oligomenorrhea include:
1. Infertility
- Anovulation (lack of ovulation) is common in women with oligomenorrhea, particularly if the condition is related to polycystic ovary syndrome (PCOS) or other hormonal imbalances. Since ovulation is necessary for pregnancy, women with irregular or infrequent cycles may have difficulty conceiving.
2. Endometrial Hyperplasia
- Endometrial hyperplasia is a condition in which the lining of the uterus becomes too thick, often due to an imbalance in estrogen and progesterone. In women with oligomenorrhea, especially those who have infrequent periods, this can occur because the endometrium is not shed regularly. If left untreated, endometrial hyperplasia can increase the risk of developing endometrial cancer.
3. Osteoporosis
- Prolonged menstrual irregularities can lead to low estrogen levels, which are important for maintaining bone density. In women with oligomenorrhea, especially if associated with conditions like anorexia or extreme exercise, low estrogen levels can contribute to osteoporosis or an increased risk of bone fractures.
4. Cardiovascular Disease
- Some studies suggest that women with conditions causing oligomenorrhea, such as PCOS, may have an increased risk of developing cardiovascular diseases. This may be related to metabolic disturbances like insulin resistance, which is common in PCOS and other causes of oligomenorrhea. Insulin resistance can lead to high blood pressure, high cholesterol, and other risk factors for heart disease.
5. Metabolic Issues
- Women with oligomenorrhea, particularly those with PCOS, are more likely to have insulin resistance, which can lead to type 2 diabetes, obesity, and dyslipidemia (abnormal cholesterol levels). These metabolic issues can significantly affect long-term health and quality of life.
6. Psychological Effects
- The challenges of coping with irregular periods, infertility, or other symptoms like acne or hirsutism can lead to psychological distress, including anxiety, depression, and low self-esteem. These mental health issues can have a significant impact on overall well-being.
7. Increased Risk of Miscarriage
- If a woman with oligomenorrhea is able to conceive, she may face a higher risk of miscarriage. This is particularly true if the oligomenorrhea is linked to conditions that disrupt ovulation or lead to poor egg quality, such as PCOS or hypothalamic dysfunction.
8. Chronic Pelvic Pain
- Women with oligomenorrhea may experience chronic pelvic pain, particularly if the condition is related to ovarian cysts or endometriosis. Chronic pain can affect quality of life and may require medical intervention.
9. Complications in Pregnancy
- For women who do conceive with underlying oligomenorrhea, there may be an increased risk of pregnancy complications. These could include gestational diabetes, hypertension, or other issues related to poor hormonal regulation or pre-existing metabolic problems.
10. Irregular Uterine Bleeding
- If ovulation does not occur regularly, women may experience unpredictable or heavy bleeding, which can lead to anemia due to prolonged or excessive blood loss.
MANAGEMENT :
general approaches to managing oligomenorrhea:
1. Lifestyle Modifications
- Diet and Exercise: If the oligomenorrhea is linked to excessive weight gain, obesity, or extreme exercise, lifestyle modifications are crucial.
- Weight Management: Achieving and maintaining a healthy weight can help regulate menstrual cycles, especially in conditions like PCOS or hypothalamic amenorrhea.
- Moderate Exercise: If excessive exercise is contributing to oligomenorrhea, reducing the intensity or duration may restore regular cycles.
2. Hormonal Treatments
Hormonal treatments can help regulate menstrual cycles and balance hormone levels.
- Oral Contraceptives (Birth Control Pills): These can regulate the menstrual cycle by providing stable levels of estrogen and progesterone. This is especially useful in women with PCOS or other hormonal imbalances. The pill can also help reduce symptoms like acne and hirsutism.
- Progestin Therapy: For women with infrequent periods due to endometrial hyperplasia or those who don’t wish to use estrogen-based contraceptives, progestin-only treatment (such as medroxyprogesterone) may be used to induce menstrual bleeding and prevent the risk of uterine cancer.
- Clomiphene Citrate: If fertility is a concern and anovulation is the cause of oligomenorrhea, clomiphene citrate may be prescribed to stimulate ovulation, particularly in women with PCOS.
- Estrogen Therapy: In women with low estrogen (such as in premature ovarian insufficiency), estrogen replacement therapy may be used to regulate cycles and prevent complications like osteoporosis.
3. Treatment for Underlying Conditions
If oligomenorrhea is due to an underlying medical condition, such as hypothyroidism or PCOS, addressing the root cause is crucial.
- Hypothyroidism: Treatment with thyroid hormone replacement (e.g., levothyroxine) can restore normal hormonal balance and menstrual regularity.
- PCOS: Along with oral contraceptives, metformin (an insulin-sensitizing drug) may be prescribed to improve insulin resistance, regulate menstrual cycles, and reduce the risk of metabolic complications.
- Hyperprolactinemia: If elevated prolactin is the cause, medications like bromocriptine or cabergoline can be used to lower prolactin levels and restore normal cycles.
4. Ovulation Induction
For women with anovulation (no ovulation), particularly those trying to conceive, medications to stimulate ovulation are commonly used:
- Clomiphene Citrate: As mentioned earlier, this medication is often the first-line treatment to induce ovulation in women with PCOS or other ovulatory disorders.
- Letrozole: Another medication used for ovulation induction, particularly in women with PCOS.
- Gonadotropins: In some cases, injectable gonadotropins (hormones that stimulate the ovaries) may be prescribed if oral medications are ineffective.
5. Treatment of Endometrial Hyperplasia
If oligomenorrhea has led to endometrial hyperplasia (thickening of the uterine lining), it may need treatment to prevent progression to endometrial cancer.
- Progestin therapy: Progestin can be used to regulate the endometrial lining and prevent overgrowth.
- D&C (Dilation and Curettage): In some cases, a D&C procedure may be performed to remove the thickened endometrial lining.
6. Surgical Interventions
- Ovarian Drilling: In cases of PCOS that do not respond to other treatments, laparoscopic ovarian drilling can be performed. This surgery involves making small holes in the ovaries to reduce androgen levels and promote ovulation.
- Hysterectomy: In rare cases where other treatments are ineffective, and the patient is not concerned about fertility, a hysterectomy (removal of the uterus) may be considered, especially if there are severe, unresolved issues with endometrial hyperplasia or cancer.
7. Monitoring and Follow-up
- Regular follow-up visits are essential to monitor the effectiveness of treatment and make adjustments as needed.
- Ultrasounds or blood tests to monitor hormone levels, the thickness of the endometrial lining, ongoing management.
- In women undergoing treatment for fertility, tracking ovulation with home ovulation predictor kits or through blood tests to check progesterone levels may be used.